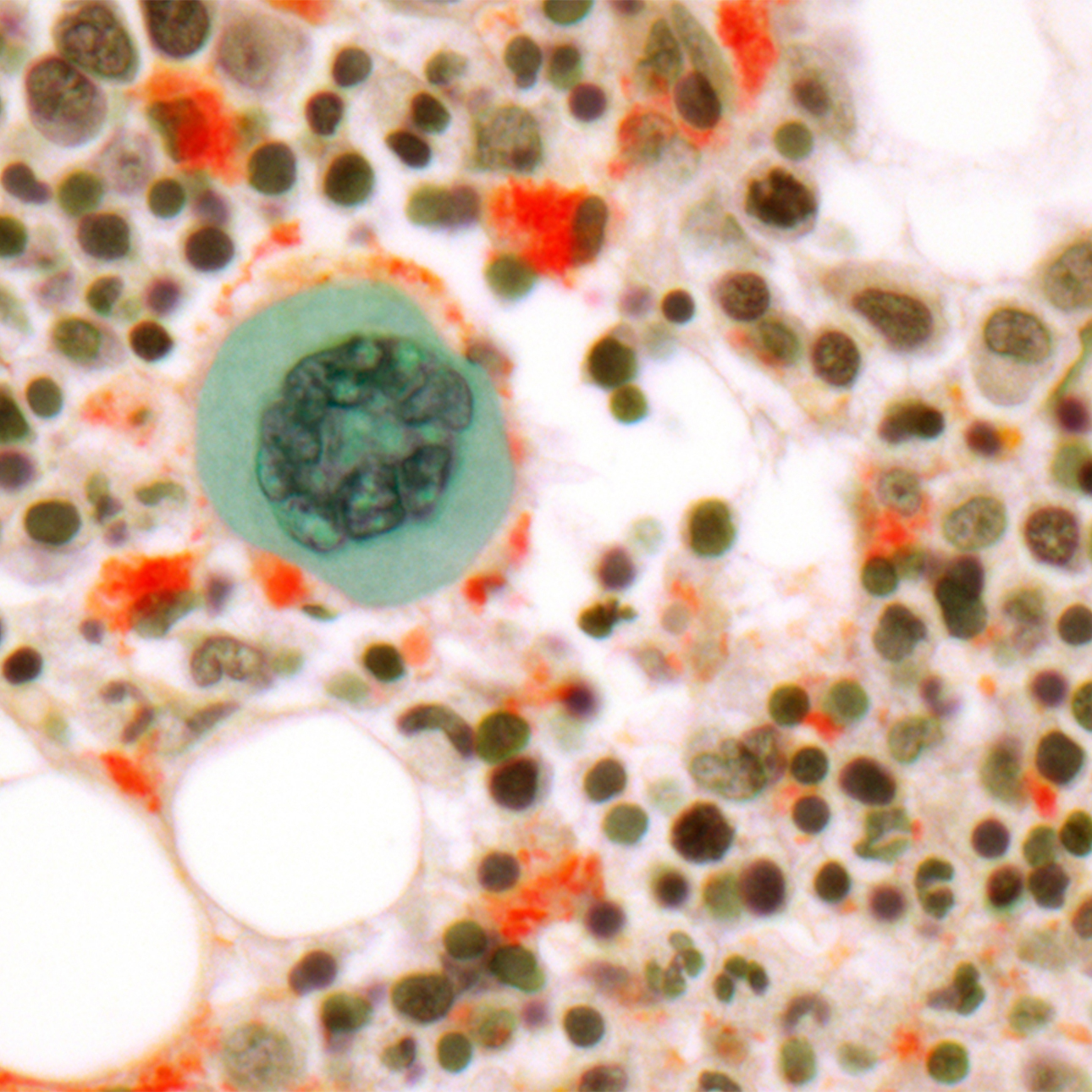
Non-Hodgkin's Lymphoma
Treatments
The treatment of non-Hodgkin's lymphoma will vary according to the specific sub-type of lymphoma.
Patients with non-Hodgkin's lymphoma undergo an extensive evaluation that may include:
- A general history and physical examination
- Multiple blood tests
- X-Rays
- Bone marrow aspiration and biopsy procedure
- Lymph node biopsy
Some slow growing lymphomas, called indolent or low-grade lymphomas, may not require any initial therapy, and the doctor may decide to wait until the disease causes symptoms before starting treatment. Often, this approach is called "watchful waiting."
That said, the majority of patients with non-Hodgkin's lymphoma will require treatment at the time of diagnosis. Treatment usually consists of chemotherapy, although some patients may receive radiation therapy, or a combination of these treatments. In some cases, bone marrow transplantation, biological therapies or surgery may be considered.
Chemotherapy
Chemotherapy is the use of drugs to kill cancer cells. Chemotherapy for non-Hodgkin's lymphoma usually consists of a combination of several drugs. Patients may receive chemotherapy alone or in combination with radiation therapy.
Chemotherapy usually is given in cycles: a treatment period followed by a recovery period, then another treatment period and recovery period, and so on.
Although most anticancer drugs are given by injection into a blood vessel (through an IV), some are given by mouth. Chemotherapy is a systemic treatment because the drugs enter the bloodstream and travel throughout the body.
The most common therapy for non-Hodgkin's lymphoma is called R-CHOP and consists of four different chemotherapy medications plus a type of immunotherapy called rituximab, which specifically targets some lymphoma cells. The medications are given through an IV and by mouth for five consecutive days. This is then repeated every three weeks for six to eight cycles.
Chemotherapy is usually an outpatient procedure, which means it can be given at the hospital, at the doctor's office or at home. However, depending on the patient's general health, a short hospital stay may be required.
Radiation Therapy
Radiation therapy, also called radiotherapy, is the use of high-energy rays to kill cancer cells. Treatment with radiation may be given alone or with chemotherapy.
Radiation therapy is local treatment, meaning it only affects cancer cells in the treated area. Radiation therapy for non-Hodgkin's lymphoma comes from a machine that aims the high-energy rays at a specific area of the body. There is no radioactivity in the body when the treatment is over.
Stem Cell Transplants
At UCSF Medical Center, stem cell transplantation, also called bone marrow transplantation, is offered to all patients with recurrent non-Hodgkin's lymphoma. The type of stem cell transplant will depend on a number of factors including:
- Age
- Current symptoms
- Response to prior treatments
- The availability of a donor
The majority of patients will undergo an autologous stem cell transplant, which uses one's own stem cells. You are encouraged to consult with a stem cell transplantation doctor to learn more about non-Hodgkin's lymphoma, including treatments and stem cell transplantation.
Stem cell transplantation refers to the administration of high-dose chemotherapy followed by the infusion of stem cells. If the stem cells are collected from the hip bone, the procedure is called a bone marrow transplant. If the stem cells are collected from the blood using a procedure called leukapheresis, the procedure is called a peripheral blood stem cell transplant. Today, most transplantation procedures are performed using stem cells that have been collected from the peripheral blood.
Peripheral stem cell transplantation is a method of giving high-dose chemotherapy and then replacing the blood-forming cells destroyed by chemotherapy with healthy stem cells.
Transplantation may be:
- Autologous — Using an individual's own blood cells that were saved earlier
- Allogeneic — Using blood cells donated by someone else
- Syngeneic — Using blood cells donated by an identical twin
Biological Therapy
Biological therapy, also called immunotherapy, is a form of treatment that uses the body's immune system, either directly or indirectly, to fight cancer or to lessen the side effects that can be caused by some cancer treatments. It uses materials made by the body or in a laboratory to boost, direct or restore the body's natural defenses against disease.
The drug rituximab is an example of one type of immunotherapy that is widely used. Newer, investigational immunotherapies and agents that are designed to enhance normal cell-death pathology, which is often inhibited in cancer cells, are currently being investigated.
UCSF Health medical specialists have reviewed this information. It is for educational purposes only and is not intended to replace the advice of your doctor or other health care provider. We encourage you to discuss any questions or concerns you may have with your provider.
Treatments we specialize in
-
Allogeneic Transplant
In a procedure similar to a simple blood transfusion, the patient receives bone marrow or stem cells from a tissue-matched donor.
Learn more -

Autologous Transplant
Stem cells collected from the blood before chemotherapy or radiation are returned to the patient's body using a process similar to a blood transfusion.
Learn more





















